In a hospital, some of the most important resources are beds and specialized nurses in the ICU, where doctors and nurses use advanced technology to save the lives of critically ill patients. But providing that sort of care is complex and expensive, and hospitals can afford to have only a limited number of ICU beds. That shortfall became tragically apparent during the COVID-19 pandemic, when some facilities ran out of capacity to deal with the large number of desperately sick patients. Even in less dire times, doctors still are compelled to make difficult choices, because they can only transfer so many patients to the ICU. At the same time, if they wait until a patient’s health deteriorates to the point where a sudden, unplanned transfer is required, patients’ chances of survival plummet.
But what if doctors had a way to reliably identify the patients whose health was most likely to take a turn for the worse, and proactively send those patients to the ICU? A 2018 research article, relying on nearly 300,000 hospitalizations in the Kaiser Permanente Northern California, provides evidence that proactively transferring patients to the ICU can significantly reduce the mortality risk and length of hospital stays. But there is a risk of going too far. Indeed, other research indicates that if doctors transfer too many patients to the ICU, the ICU may become congested and the survival rate is negatively impacted. In a worst-case scenario in which the ICU is filled to capacity, this could mean that some patients who need ICU care are not able to obtain it.
For a proactive ICU transfer policy to work, three variables are needed: to recalibrate depending upon arrival rates during the day and night, how many nurses you have in the ICU, and whether transferred patients are recovering fast enough. If these metrics are not aligned, you might not make the right transfer decisions.
What we learned by using data to create a simulated hospital
One of my esteemed collaborator, Gabriel Escobar, served as the regional director for hospital operations research at Kaiser Permanente North California in the United States. That provided us with a great opportunity to work with anonymized hospitalization data on 300,000 patients from 21 Kaiser Permanente facilities. We had a tremendous amount of detailed data on cases, right down to things like blood cell counts taken every six hours. Based upon this data, we were able to estimate things such as how patients react to different treatments and various arrival and admission rates to the ICU and the common ward.
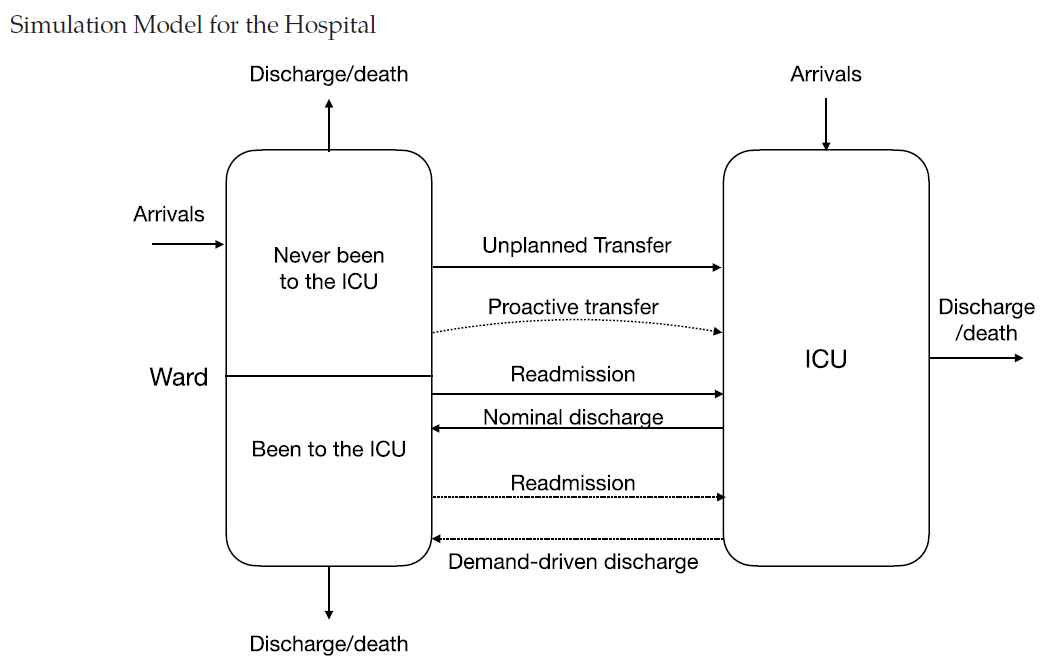
With all this information, we were able to build a simulation model, which mimics how an actual hospital works, such as generating arrival and departure rates, the evolution of the patients and every single interaction they have with the system. With this sort of micro-modeling, you can track the simulated patient like you would a real patient during their journey in the hospital. This enables to test different scenarios of arrivals and transfer policies.
In doing our study, we utilized a mathematical model called a Markov Decision Process model, which often is used in AI. In plain English, an MDP is a natural model for sequential decision-making, in which you can inspect a sequence of decisions, and how one choice influences the next one and the overall health outcome. The sequence is influenced only by earlier decisions, not by what you might do down the line--what happens at noon, for example, isn’t affected by what will happen at 3 p.m., because that hasn’t happened yet. But you are influenced by what happened at 9 or 10 or 11 a.m.
The goal is to make the best decisions, not only for each patient but also with the best overall result, that is, the best outcome over the general patient population. We are concerned about the survival of the patient, and at the same time, we want to maintain the ICU occupancy at a reasonable level, so that others do well, and so that unplanned transfers may still be accounted for. We designed an optimization method, based upon machine learning model, to estimate the impact of various transfer policies.
When we ran the model, one surprise was that relatively small adjustments can have a big effect on the mortality of the overall patient population.
When we ran the model, one surprise was that relatively small adjustments in the number of health resources that the system consumes and in the arrival and recovery rates can have a big effect on the mortality of the overall patient population. Given a certain way of transferring patients, we could see the estimated mortality could jump by 20 %.
AI won’t replace human decision making in hospitals
Some people might think that the questions is whether humans should make the decisions about ICU transfers, even though they sometimes make mistakes, or whether algorithms should do it. But as I see it, these two methods are really complementary. At least in the foreseeable future, humans will have the last word. But they are more likely to make those decisions assisted with the recommendations of an algorithm. We want it to be the best automated recommendation system, and it has to provide interpretable insights on its recommendation. If the practitioners are not able to understand where the recommendations come from, they will never use it.
We have to go back the question: what exactly is at stake here? If one patient is transferred to an ICU bed, the patient has better treatment and more nursing, and better survival chance. But at the population level, if the patient transfer is going to cause the ICU to be congested, this becomes a problem for everyone else. What we are doing in this work is to look for simple transfer decision rules, based on common health metrics summarizing the health conditions of the patients and certain thresholds. This type of threshold policy is extremely simple to deploy and readily interpretable.
Using micro-modeling to understand a complicated enterprise and develop algorithms to assist in decision making can lead to better outcomes.
How to Use the Insights: Using micro-modeling to understand a complicated enterprise and develop algorithms to assist in decision making can lead to better outcomes. But it also requires an understanding of variability, and how relatively small changes in the conditions can significantly alter outcomes. Ultimately, it is up to the doctors to make the transfer decisions, but machine learning models may help to assist in the decisions and to provide valuable information regarding the impact of patient transfers.